The role of hormones in your menstrual cycle
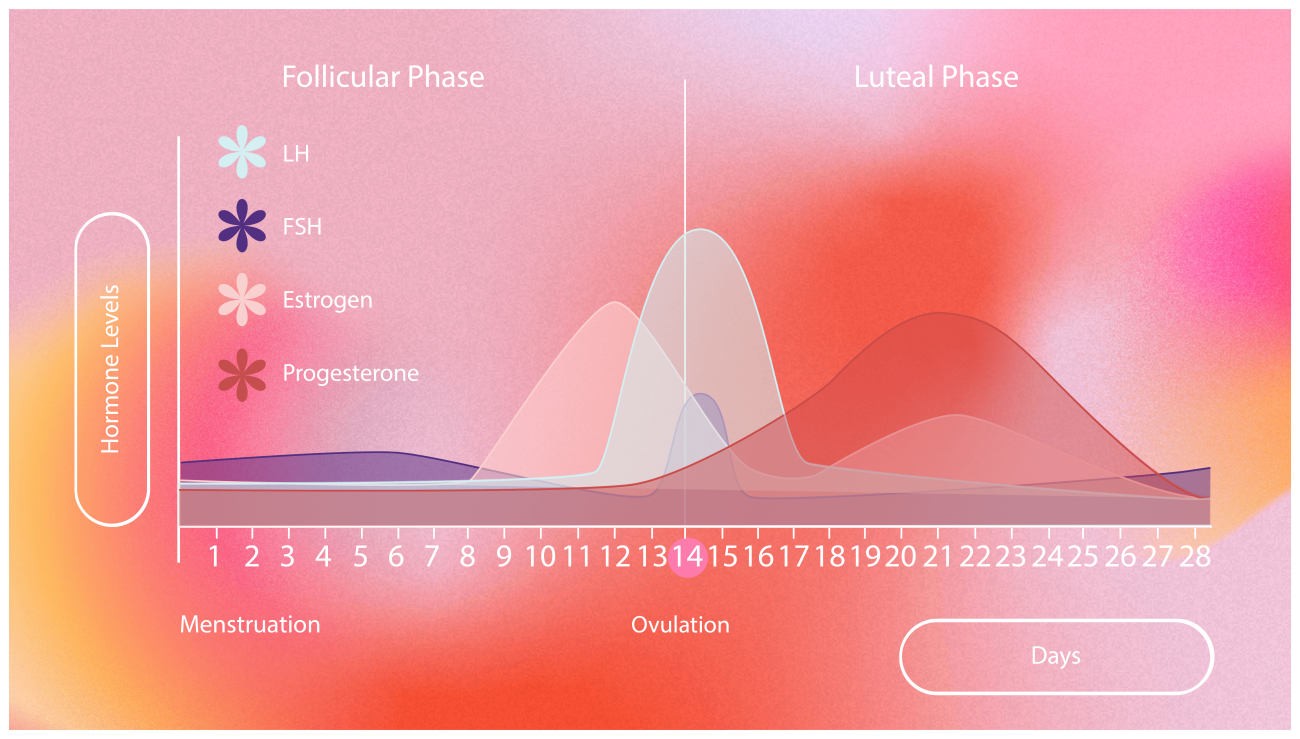
Your menstrual cycle is regulated by fluctuating menstrual cycle hormones such as oestrogen and progesterone. Understanding how these hormones shift during each period cycle phase can help you track symptoms, manage fertility, and feel more in control of your body.
And if your timing’s a little off? No stress.
Ever feel like your body’s on a schedule you didn’t choose? That’s your menstruation cycle, powered by a clever hormone system. If you’re managing PMS, planning a pregnancy, or simply curious about your normal period cycle, learning how hormones fluctuate in each phase helps you feel more connected to your reproductive health.
What is the menstrual cycle?
Your menstrual cycle is more than just your period. It’s a monthly hormonal process your body goes through to prepare for pregnancy. A typical cycle lasts 21–35 days and includes four key phases:
1. Menstrual phase
2. Follicular phase
3. Ovulation
4. Luteal phase
Each of these phases is controlled by shifting levels of key hormones like oestrogen, progesterone, LH (luteinising hormone), and FSH (follicle-stimulating hormone).
Phase by phase: How hormones shape your cycle?
1. Menstrual phase (Day 1–5)
Your cycle starts with your period. If no pregnancy occurred in the previous cycle, your uterus sheds its lining. That’s your menstrual bleeding.
– Hormones involved: Oestrogen and progesterone levels are low
– What happens: Shedding of the uterine lining
– You might feel: Fatigue, cramping, or emotional shifts
2. Follicular phase (Day 1–13)
This overlaps with your period and continues until ovulation. Your brain sends signals (via FSH) to your ovaries to mature a follicle, which holds an egg.
– Hormones involved: Rising oestrogen, FSH
– What happens: Uterine lining starts rebuilding; one dominant follicle matures
– You might feel: A boost in energy and mood as oestrogen rises
3. Ovulation (Around Day 14)
Oestrogen hits a peak, triggering a surge of LH. This causes the dominant follicle to release its egg. This is your fertile window.
– Hormones involved: LH surge, peak oestrogen
– What happens: Egg is released into the fallopian tube
– You might feel: Mild cramps (mittelschmerz), increased libido, egg-white cervical mucus
4. Luteal phase (Day 15–28)
The released follicle turns into the corpus luteum, which pumps out progesterone to prepare the uterus for pregnancy. If fertilisation doesn’t happen, hormone levels drop, triggering your next period.
– Hormones involved: Progesterone (dominates), declining oestrogen if no pregnancy
– What happens: Uterus prepares for pregnancy, then resets
– You might feel: PMS symptoms like bloating, breast tenderness, irritability
What happens when hormones are out of sync?
Hormonal imbalances1can throw off your menstrual cycle. Irregular periods, heavy bleeding, missing periods, or severe PMS might point to:
– PCOS (polycystic ovary syndrome)
– Thyroid dysfunction
– Endometriosis
– Stress or extreme weight changes
If your cycle seems off for more than a couple of months, speak to your doctor. They may recommend hormone testing or cycle tracking tools to find out what’s going on.
Can I track my hormones at home?
Absolutely. Many people now use fertility tracking apps and ovulation predictor kits to better understand their cycles. These tools help you:
– Identify your fertile window
– Recognise hormonal shifts
– Understand symptoms like cramps or mood swings
Need backup birth control? We’ve got you
Even when you’re tuned into your cycle, ovulation doesn’t always follow a script. If you had unprotected sex or a birth control mishap, emergency contraception like ellaOne can ease your mind. It works by delaying ovulation, so no egg is released, meaning no fertilisation.
And don’t worry: ellaOne is unlikely to affect your long-term fertility or mess up your hormone balance.
Summary
Your menstrual cycle is driven by hormones that rise and fall in a natural rhythm, controlling ovulation and your period. When balanced, they keep your cycle regular and reproductive health strong. Understanding them helps you take charge of your body.
FAQ
1. What are the roles of hormones in the menstrual cycle?
Oestrogen, progesterone, LH, and FSH regulate your menstrual cycle. They control the release of an egg (ovulation), thicken the uterine lining, and trigger your period when pregnancy doesn’t occur.
2. How do hormones change during each period cycle phase?
– Menstrual phase: Oestrogen and progesterone drop, sparking your period
– Follicular phase: Oestrogen and FSH rise to mature a follicle
– Ovulation: LH surge releases the egg
– Luteal phase: Progesterone rises to prepare for pregnancy, then drops if fertilisation doesn’t occur
3. What are symptoms of low oestrogen?
If you’re low on oestrogen, you’ll likely experience hot flashes, night sweats, mood changes, vaginal dryness, and irregular periods.
4. What are signs of low progesterone?
Low progesterone cause irregular periods, spotting, fatigue, low libido, and mood swings, especially in the second half of your cycle.
5. What is the luteal phase and why is it important?
The luteal phase is the second half of your cycle, post-ovulation. Progesterone dominates to prepare your body for pregnancy. If levels are too low, it can affect fertility and cause PMS symptoms.
6. How can I check my hormone levels at home?
You can use hormone testing kits, track basal body temperature, or monitor symptoms like cervical mucus. If you’re unsure, consult a healthcare provider for lab testing.
ellaOne® 30mg film-coated tablet contains ulipristal acetate and is indicated for emergency contraception within 120 hours (5 days) of unprotected sexual intercourse or contraceptive failure. Always read the label.
*Verify at ellaone.co.uk/verify